The ability to look inside the body without the need for explorative surgery is a key component to modern medicinal practice. Not only does it make it easier for practitioners to get a better idea of what is happening inside a patient’s body, it’s also far less invasive and uncomfortable for the patients themselves. But what’s the origin of this ability to look inside the body? Well it all began in the late 19th century with a man named Röntgen…
Who was Röntgen?
At the end of the 1800s, many physicists were studying the conduction of electricity. One of them was Wilhelm Röntgen, a 50-year-old professor of physics at Würzburg University in Germany, who was investigating electrical conduction through gases. He applied a very high voltage across an evacuated glass tube, trying to get the electric current to come out through a thin aluminium window. In November 1895 he noticed that a fluorescent screen in his laboratory glowed when the tube was activated. This chance observation led him to the discovery that a new sort of radiation, which he called X-rays, was being produced.
When his discovery was announced in January 1896, the world was astonished. Physicists tried to understand the nature of the new rays. Rumours spread that they would allow anyone to spy through closed doors. But one picture in particular set the medical world alight. This was the image of the left hand of his wife, showing clearly the bones and joints of her fingers and her ring. Doctors scrambled to find out more, to get hold of equipment, to look inside their patients and themselves.
X-rays in Bath
By February, Bath citizens were able to see X-rays demonstrated, first by James Gifford, owner of a lace-making factory from Chard, Somerset, and amateur scientist. Gifford subsequently helped arthritis doctors at the Royal Mineral Water Hospital and used X-rays to show the causes of deformity. Then, Bath scientific instrument maker John Rudge gave two practical demonstrations of ‘electrical shadow photography’. Rudge’s well-publicised inventions included intense outdoor lighting, artificial aurora-borealis and an electric model railway. His work with William Friese-Greene on the Biophantascope is remembered by a plaque in New Bond Street Place. Rudge soon examined two patients from the Royal United Hospital (RUH), locating a needle in the hand of one and detecting a bullet embedded in the finger of another. Rudge offered a new service allowing Bath doctors to look inside their patients’ bodies.
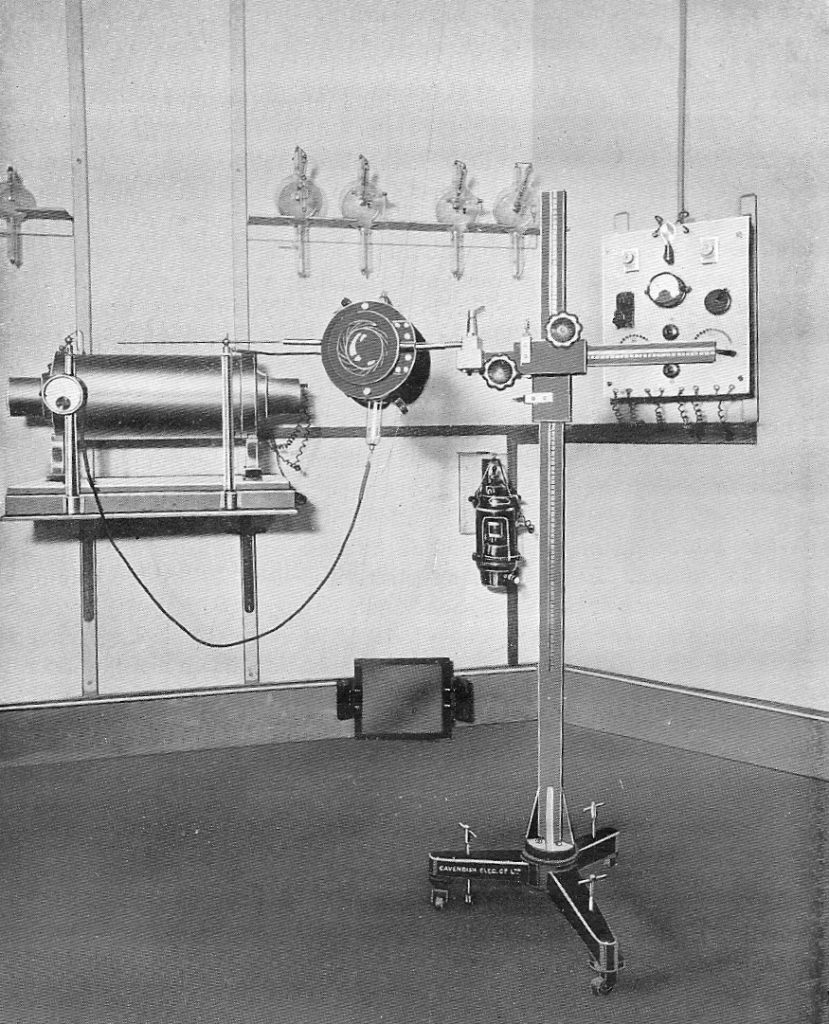
In 1901 Rudge supplied the components for the first X-ray equipment at the RUH, costing £30; coil, tubes, battery and fluorescent screen. The first radiologist was Preston King, later twice Mayor of Bath, who led radiology in Bath throughout his career.
Early X-ray equipment needed regular attention because the output changed. The electrons that produced X-rays by bombarding the anode were produced by gas ionisation, so the vacuum changed. The high-vacuum Coolidge tube was developed later, in 1912, and was more stable because the electrons were released by heating a fine metal coil. After the First World War, high voltage equipment using Coolidge tubes gave sufficient energy to penetrate through the thickest parts of the body, seeing inside the abdomen as well as through the chest and limbs. Many other improvements ensued, including better resolution, electronic fluoroscopy, shorter exposure times and, eventually, the replacement of photographic film with digital detection.

The problems with x-rays
X-rays work because they are stopped by bone, forming shadows. X-rays pass very easily through the air in the lungs, giving an ‘inverse shadow’. But the rest of the tissues in the body, muscle, liver, brain and blood, produce more or less the same shadow. Contrast agents had to be used to show blood flow and the working of the intestines and kidneys. In addition, an X-ray image does not distinguish between deep and shallow tissues. New ways of looking inside the body were needed.
The other difficulty with using X-rays is that they can be dangerous. Lead sheets were wrapped around X-ray tubes, and lead-rubber gloves and aprons were supplied, to limit the exposure to radiologists and technicians. In the early days, when few X-rays were carried out, these precautions were mostly sufficient. But there was a huge expansion of military radiology during the First World War, often carried out by untrained staff using cheap unsafe equipment. By the end of the war, many doctors and radiographers were suffering from chronic effects to their hands, which for many became cancerous. Some developed leukaemia. Those who died are commemorated in the X-ray Martyrs’ memorial in Hamburg.
New ways of imaging
Ultrasound
60 years after X-rays first saw inside the body, new methods started to emerge. Ultrasound imaging could show depth. The NHS began to install British-made ultrasound scanners for baby scanning in the 1960s. They worked like underwater SONAR, making images using echoes of ultrasound pulses. At first the images were very difficult to interpret, but the images from the first RUH scanner, installed in 1976, were much clearer, and could be used to scan for cancer as well as in pregnancy. Ultrasound is also able to image flowing blood, using the Doppler effect.
Nuclear medicine
At the same time another new imaging method, using radioactive materials, was developed. The gamma camera enabled the distribution of radioactivity in the body to be seen, following the injection of a radionuclide. The images are less clear than radiographs, but nuclear medicine is valuable because it can show how an organ is working. Thyroid and kidney function can be evaluated, secondary bone cancers can be mapped and radioactive gas can show lung ventilation. Soon, heart scanning using ultrasound and nuclear methods developed. Nuclear medicine remains a small but important specialist imaging technique, especially with the further development of positron emission tomography (PET).
Thermography
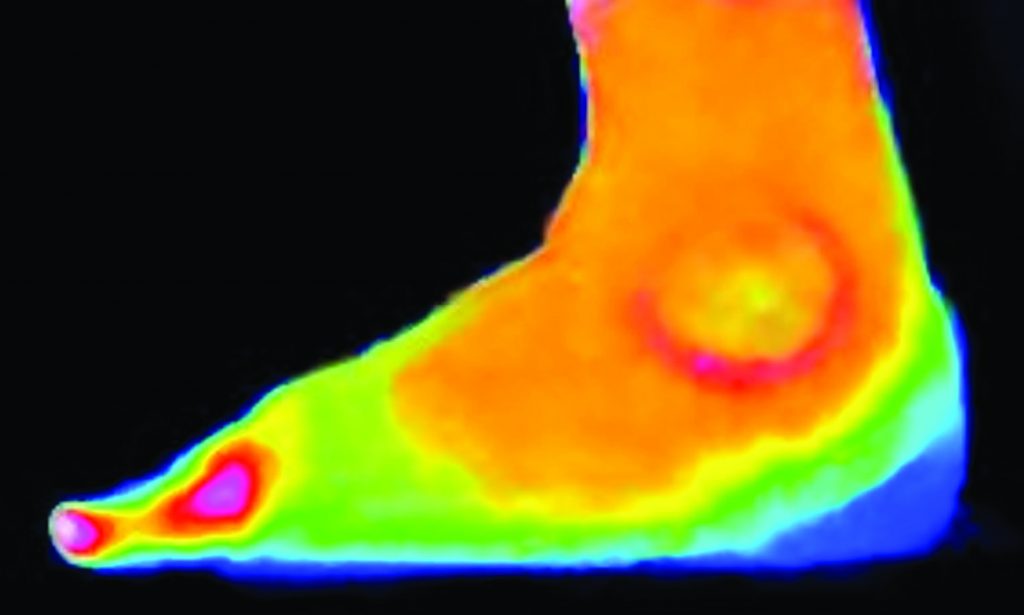
Inflamed tissues radiate heat which can be detected using thermal imaging cameras, a technique which was pioneered by Dr Francis Ring at the Royal National Hospital for Rheumatic Diseases (RNHRD) in Bath to demonstrate joint inflammation and aid in the investigation and treatment of arthritis.
Computed x-ray tomography
Computed X-ray tomography (CT) is a method of producing cross-sectional images of the body using x-rays. The first scans were made in London in 1971, using a scanner made by EMI and designed by Nobel-prize-winner Godfrey Hounsfield. Many X-ray images are made as the tube moves around the body, and the data are used to calculate the X-ray attenuation coefficient at each point in the body. In this way, soft tissues can be distinguished, individual organs can be seen, and cancers defined.
Magnetic Resonance imaging
The first magnetic resonance imaging (MRI) scanner was installed at the RUH in 1997, over a decade after the first CT scanner. MRI was developed during the 1970s and early 1980s but the purchase and running expenses limited its early implementation. MRI works by causing hydrogen atoms in the body to absorb electromagnetic energy at a frequency set by a high magnetic field, and then detecting the small radiofrequency signal that is given off. It is even better than CT at imaging soft tissue, although not as effective at imaging bone as X-rays, and not as cost-effective as ultrasound for dynamic imaging.
Conventional X-ray imaging still constitutes about half of medical imaging. Ultrasound now contributes about a quarter of all scans, followed by CT and MRI.
Article by Prof. Francis Duck M.B.E